Helping Avoid Intubation in Complex COVID-19 Patient Through Inhaled Epoprostenol via High Velocity Aerosol Circuit
Jeremy Greenberg, MD
Disclaimer: Vapotherm’s high velocity therapy is a tool for treating respiratory distress. Although individual results may vary, Vapotherm believes this case study is an example of the clinical benefit Vapotherm’s high velocity therapy can have on patient ambulation. Practitioners should refer to the full indications for use and operating instructions of any products referenced herein before prescribing them.
A 61-year-old male with a history of essential hypertension, hyperlipidemia, and chronic kidney disease (CKD) stage III was admitted to the intensive care unit (ICU) with sepsis, acute respiratory distress syndrome (ARDS), and acute kidney injury (AKI) on CKD due to infection with SARS-CoV-2.
The patient had been in his normal state of health until 2 days prior to this admission, when he developed gradual onset, progressively worsening dyspnea prompting a visit to his local emergency department. He described his dyspnea as moderate intensity and worsened by exertion. He also had associated symptoms of a non-productive cough, fatigue, and change in his usual taste and smell. He had no fever, chills, chest pain, or gastrointestinal symptoms. His wife had tested positive for SARS-CoV-2 four days prior. His home medications included Atorvastatin, Omeprazole, Losartan, Tamsulosin, and Veltassa. His temperature was 99.2°F (37.3°C), the heart rate 92 beats per minute, the blood pressure 89/55 mmHg, the respiratory rate 16 breaths per minute, and the oxygen saturation (SpO2) 87% while breathing ambient air. He appeared ill but not toxic. He was speaking in full sentences and had normal work of breathing. His lungs were clear to auscultation bilaterally. The remainder of his physical exam was reassuring.
Laboratory evaluation revealed a normal white blood cell count (WBC), normal hemoglobin (Hgb), and normal platelet count (Plt). A comprehensive metabolic panel showed a normal sodium, potassium, chloride, and glucose. His blood urea nitrogen (BUN) and creatinine (Cr) were elevated at 56 and 3.9, respectively. His bicarbonate was 15 and his anion gap 14. An arterial blood gas showed a pH of 7.36, a partial pressure of carbon dioxide (PaCO2) of 29 mmHg, and a partial pressure of oxygen (PaO2) of 59 mmHg. Testing for SARS-CoV-2 was positive. Chest x-ray was reported as negative for acute pathology.
Blood cultures, respiratory cultures, and respiratory viral panel were obtained. He was given 1L of normal saline and received levofloxacin for suspected community acquired pneumonia. His hypoxemia was managed with supplemental oxygen with a nasal cannula (NC) at 2 liters per minute (L/min). He was admitted to the hospital ward.
The inpatient hospitalist team continued therapy with supplemental oxygen. He was additionally started on hydroxychloroquine and zinc. The following day his SpO2 was 88% on 11 L/min of oxygen via NC. Laboratory evaluation showed worsening BUN and Cr. The inpatient team elected to transfer the patient to our referral center for respiratory support and evaluation for renal replacement therapy. He was transferred via EMS to our non-ICU COVID-19 ward.
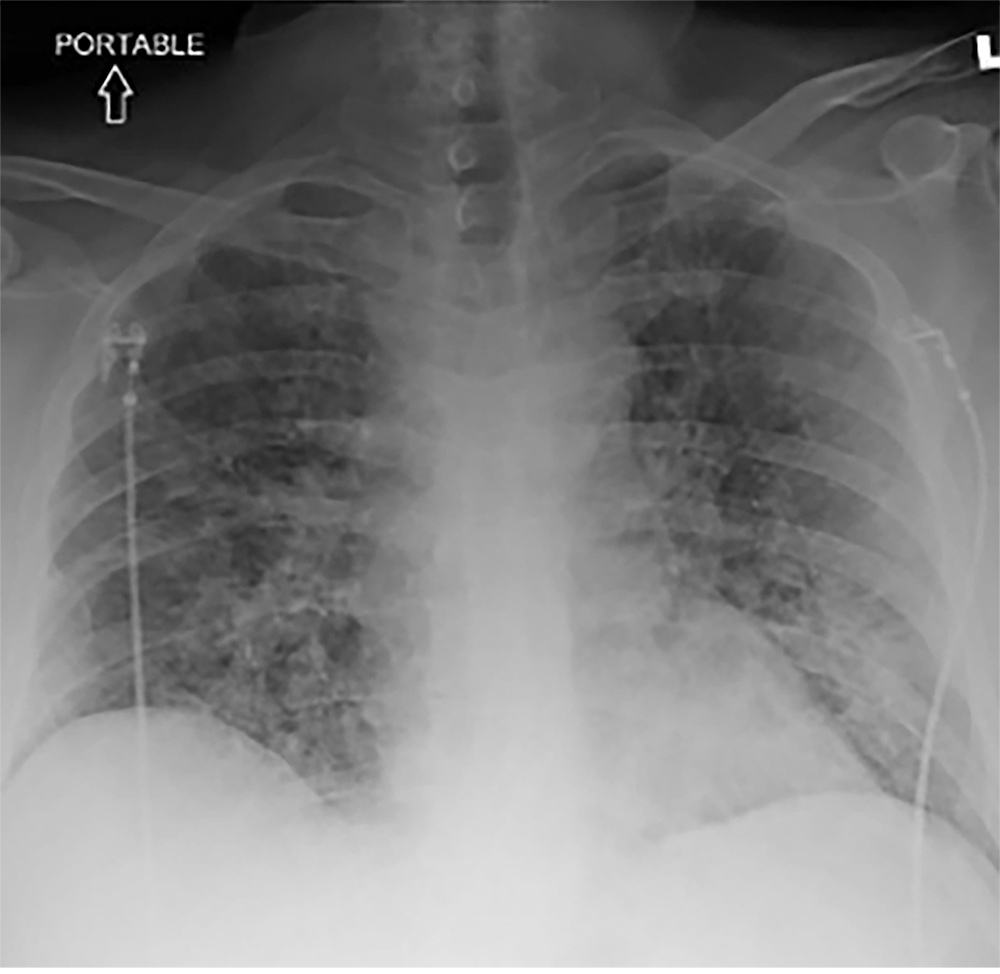
Shortly following arrival, his SpO2 had decreased to 83% on a reservoir non-rebreather mask at flush rate oxygen and the critical care medicine team was emergently consulted. Assessment by the critical care medicine team revealed his heart rate was elevated to 131 beats per minute, the blood pressure 105/48 mmHg, the respiratory rate 44 breaths per minute (bpm), and the oxygen saturation 83%. He was in extremis and communication was limited to single word sentences. He had sternal retractions with inspiration. Crackles were heard on bilateral lung auscultation. A repeat arterial blood gas showed a pH of 7.32, PaCO2 34 mmHg, PaO2 of 46 mmHg. A chest x-ray showed bilateral, multifocal, patchy airspace disease (see Figure 1).
A point-of-care ultrasound showed a thick-walled left ventricle with hyperdynamic function, a right ventricle that was normal in size and function, an inferior vena cava that was < 1.5 cm with greater than 50% respiratory variability and bilateral B-lines in all imaged lung fields. Due to rapidly progressive acute respiratory failure, he was moved to a negative pressure room in the COVID-19 ICU. Once there he was placed on Vapotherm high velocity therapy at a flow of 40 L/min and a fraction of inspired oxygen (FiO2) of 60%. His respiratory rate improved to 34 bpm and his SpO2 to 91% though he remained ill appearing. Repeat laboratory assessment was obtained. A CBC again showed a normal WBC, Hgb, and Plt count. A CMP showed a bicarbonate of 13, BUN of 55, and Cr of 4.1. Lactate was 3.9. Fluid resuscitation with serial 500 mL boluses of lactated ringers was administered until his tachycardia improved, shock index resolved, and capillary refill time was < 3 seconds. He was started on Decadron, his antibiotics were continued, and his hydroxychloroquine was discontinued.
He spent the subsequent two days receiving respiratory support with high velocity therapy at the above settings. During this time, his RR ranged from 28-36 and SpO2 88-93%. His vital signs were otherwise within normal limits. His BUN improved to 29 and Cr to 2.5, both consistent with his most recent pre-admission renal biomarker profile and it was felt that he would not require renal replacement therapy. He was unable to self-prone due to back and neck pain. He received convalescent plasma as part of an investigational study. He was not given Remdesivir due to AKI on CKD. Culture data from his local hospital was negative for bacterial co-infection and serial procalcitonin levels were within normal limits and so his antibiotics were discontinued.
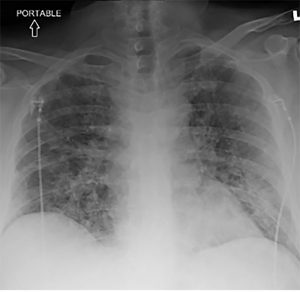
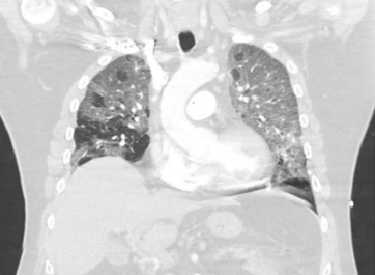
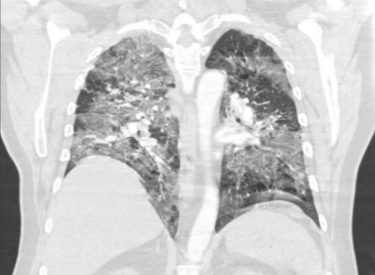
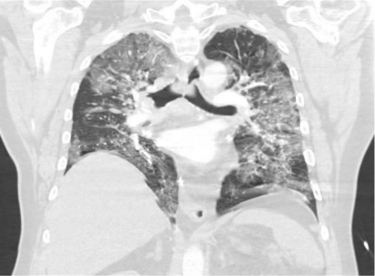
On ICU day 3, he developed increased work of breathing. His RR returned to 44 bpm and his SpO2 dropped to 84%. High velocity therapy settings were adjusted to 40 L/min and 100% FiO2. His respiratory parameters and gas exchange showed only minimal improvement. A non-rebreather mask with reservoir was placed over the high velocity therapy cannula due to the patient’s high work of breathing in an attempt to improve oxygenation by decreasing entrainment of room air. He again demonstrated only mild improvement in RR and SpO2, the latter improving to 86%. Repeat blood and respiratory cultures were obtained, as was a serum (1,3)-beta-D-glucan and a serum aspergillus galactomannan. A computed tomography pulmonary angiogram was obtained. This was negative for pulmonary embolism though showed diffuse, bilateral, ground-glass (see Figures 2-6).


He was placed on empiric, broad-spectrum antibiotics for possible healthcare associated pneumonia. The risks and benefits of intubation were discussed. The patient’s uncle had recently died while receiving mechanical ventilation related to respiratory failure from infection with SARS-CoV-2 and was apprehensive to undergo endotracheal intubation. He inquired if there were any other possible therapies. As an alternative to invasive mechanical ventilation, he was administered inhaled Epoprostenol at 30,000 ng/mL via the aerosol disposable patient circuit with high velocity therapy. His RR decreased to 28 and SpO2 increased to 95% over 10 minutes.
He remained on high velocity therapy at 40 L/min and 100% FiO2 while receiving inhaled Epoprostenol for 3 days. During this time, his RR ranged from 24 – 32 bpm and his SpO2 91-97%. The Epoprostenol was then weaned from 30,000 ng/mL to 20,000 ng/mL. His respiratory parameters remained unchanged over the subsequent 12 hours and so the dose of inhaled Epoprostenol was decreased by half every 8 hours until a dose of 2,500 ng/mL, at which point the medication was discontinued. The high velocity therapy settings were titrated over the subsequent 18 days targeting an SpO2 of 88-95%. When high velocity therapy was at 15 L/min and 25% FiO2, he was transitioned to 6 L/min via NC. All culture data was negative, and antibiotics were discontinued after 3 days of therapy. He was then transferred from the ICU to the COVID-19 ward.
He remained in the hospital for an additional 9 days. His hospitalization was complicated by hyperactive delirium requiring neuroleptic administration and deep venous thrombosis of the left lower extremity requiring systemic anticoagulation initially with Heparin infusion and then transitioned to Warfarin. He was ultimately discharged to a rehab facility still requiring supplemental O2 at 3 L/min.
He was reached by phone approximately 4 weeks following hospital discharge. He no longer required supplemental oxygen. He reported still feeling very fatigued, was experiencing reversal of his normal sleep wake cycle, and was struggling with constant “brain fog.” He also talked about how lonely he was feeling due to the prolonged duration of the pandemic. He expressed tremendous gratitude for the care he received.
While there are likely innumerable factors that contributed to this patient’s favorable outcome and survival, I believe the combination of high velocity therapy and administration of inhaled Epoprostenol via the aerosol disposable patient circuit prevented the need for invasive mechanical ventilation. While invasive mechanical ventilation has been successfully employed and expertly administered during the pandemic for countless with life-threatening, critical illness, when it can be safely avoided, as was done in this case, the risk of iatrogenesis undoubtedly decreases precipitously.