In Silico Modeling of Aerosol Generated During High Velocity Therapy Treatment

In March, 2020 Leonard and colleagues released a Transmission Assessment Report on High Velocity Nasal Insufflation (HVNI) Therapy Application in Management of COVID-19. The report includes a literature review as well as the results of computational fluid dynamics modeling (CFD)—in silico testing—to evaluate the scale of potential environmental contamination associated with aerosol generation during high velocity therapy (in the report referred to as HVNI). The authors concluded that using high velocity as a means of high flow oxygen delivery presents a low risk of transmission compared to other ventilatory support devices. Additionally, the authors found that a surgical mask applied over the high velocity cannula interface maintained therapy efficacy while effectively containing the dispersal of potentially infectious particles.
Chief Transmission Pathway of COVID-19
COVID-19 is transmitted via respiratory droplets and fomites during close unprotected contact with an infected individual.1
Risks of Transmission from High Velocity Therapy as an Aerosol Generating Procedure (AGP)
All respiratory support by its nature is an AGP, but the risk of transmission varies depending on the procedure. Based on the literature review, the authors note that “the AGP-related Severe Acute Respiratory Syndrome (SARS) transmission to Health Care Workers (HCW) only increased with tracheal intubation, NIV (by NiPPV), tracheotomy, and manual ventilation before intubation.” By comparison, there was “not a significant increase in risk for high flow oxygen therapy, manipulation of oxygen mask, endotracheal aspiration, bronchoscopy, and nebulizer treatment.”2 The authors therefore point to the need for proper interface practice (mask fitting) when it comes to NIV as well as high flow oxygen delivery (e.g. high velocity, HFNC) and note that cannula-based devices present fewer challenges for good interface practice by comparison to mask-based devices.
Computational Fluid Dynamics Modeling Scenarios
The CFD model was performed in ANSYS Fluent CFD (ANSYS, Inc, Canonsburg, PA, USA) and simulated several cases of a patient breathing at 32 bpm at a tidal volume of 500ml. Table 1 shows the breakdown of all studied scenarios. Table 1. Computational Fluid Dynamics Modeling Scenarios
Table 1. Computational Fluid Dynamics Modeling Scenarios
Results of CFD Particle Transmission During High Velocity Treatment
The testing found that with a surgical mask in place over the high velocity cannula interface captured the majority of all particles leaving the patient’s nose and mouth. The mask reduced the velocity of gas leaving the patients face significantly. (Figure 1)
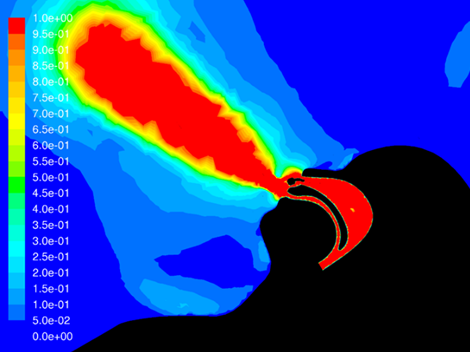
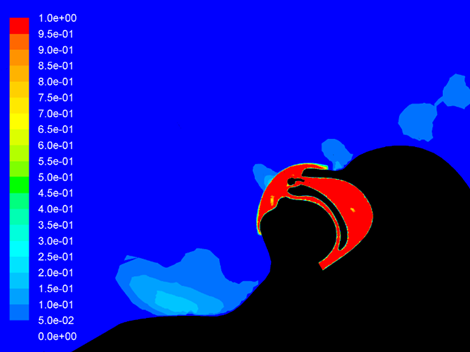
Figure 1. Particle dissemination from patient treated with high velocity without a surgical mask (left) and with a surgical mask (right)

Using the mask during high velocity therapy contained 83.2% of the particles. This was only slightly less than using a mask without treatment, where it contained 87.2% of particles. The high velocity +Mask containment was better than particle containment using a mask on low flow oxygen (73.6%). Table 2 shows the breakdown.Table 2. Comparison of Particles Caught by Surgical Mask
It’s worth noting that the most obvious particulate movement occurred via the leaks in the mask. The authors recommend minimizing mask leaks to further reduce the risk of transmission.
Impact on Therapy Efficacy with Surgical Mask
The report found that using a surgical mask with high velocity still achieved significant clearance of CO2 from the upper airway. However, the mask did lead to a 37% reduction of CO2 clearance at 35 L/min. Clinicians using high velocity for ventilatory support should consider adjusting starting flows higher because the high velocity flush is a key mechanism of achieving that ventilatory support.
Conclusion
Modeling shows that the use of a well-fit surgical mask securely placed over the properly applied high velocity cannula reduces the spread of particles down to what is comparably seen with normal breathing while wearing the mask. Surgical mask application does not eliminate the clinical efficacy of high velocity, but a higher flow setting may be required for ventilatory support.
References