Rethinking Ventilation—Do you always need pressure?
Rethinking Ventilation—Do you always need pressure?
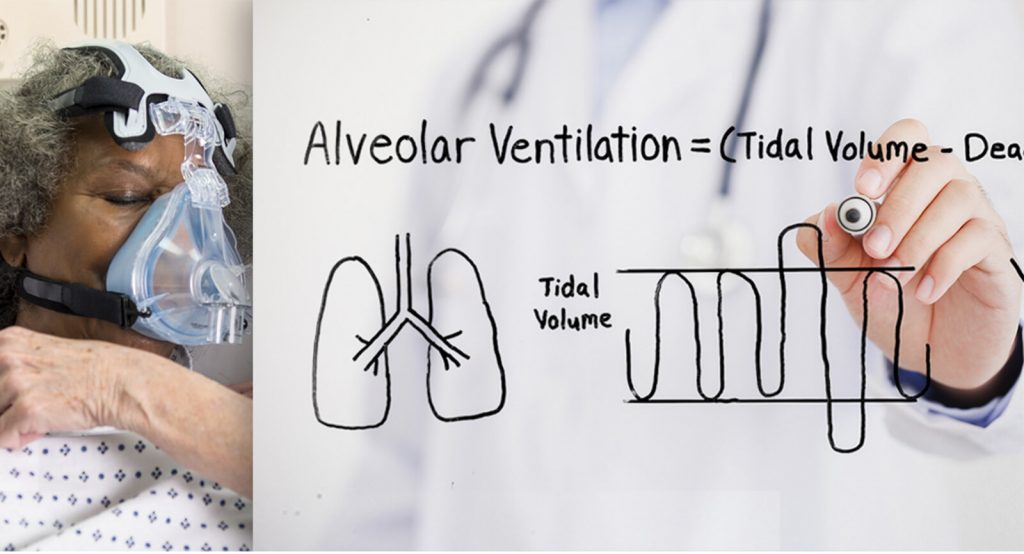
The frequent-flyer COPDer comes into the hospital, dyspneic and tripoding and the respiratory therapist is readying the non-invasive positive pressure ventilation (NiPPV)—this is a frequent sight for clinicians admitting respiratory distress patients. NiPPV has been the gold standard treatment for patients with hypercapnia. It reduces the risks associated with mechanical ventilation (MV) while also being more tolerable for the patient.11. Mehta, Sangeeta and Nicholas S. Hill. Noninvasive Ventilation. American Journal of Respiratory and Critical Care Medicine 163(2). (2001) https://doi.org/10.1164/ajrccm.163.2.9906116Read Full Text But while NiPPV may be preferable to intubation, it’s not necessarily a therapy that all indicated patients tolerate.
Whether it’s facial hair which prevents a seal, nausea that presents an aspiration risk, a patient with anxiety or severe discomfort at a tight mask-interface, NiPPV is not the solution for everyone. 12-33% of all NiPPV failure is ascribed to discomfort alone while 30-50% of patients may be intolerant.22. Carron M. et al. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. British Journal of Anaesthesia. 110(6):896-914. (2013) https://www.ncbi.nlm.nih.gov/pubmed/23562934Read Full Text These problems—tight mask seal, discomfort, difficulty to communicate or take oral hydration and medication while wearing the mask—are rooted in the need to achieve pressure as the primary mechanism of action. So, the question is: must there be pressure in order to achieve alveolar ventilation in spontaneously breathing patients?
Ventilatory Support with an Open System
Let’s review the basics:
Alveolar Ventilation = (Tidal Volume — Dead Space) x Respiratory Rate
In order to achieve ventilation, NiPPV most greatly affects the Tidal Volume aspect of the above equation.1 The machine ensures ventilation by delivering the Tidal Volume. This is accomplished with positive pressure. Because there is a risk of over-pressurization, clinicians generally start low and adjust up for effect to stabilize a patient.
However, it is also possible to achieve alveolar ventilation by affecting the other parameter in the equation: Dead Space.
Alveolar Ventilation = (Tidal Volume — Dead Space) x Respiratory Rate
The rapid flushing out of the upper airway Dead Space is the mechanism of action by which High Velocity Nasal Insufflation (HVNI) facilitates alveolar ventilation.3,43. Dysart K, Miller T, Wolfson M, Shaffer T. Research in high flow therapy: Mechanisms of action. Respiratory Medicine. 2009; 103: 1400-05Read Full Text
4. Miller TL, Saberi B, Saberi S (2016) Computational Fluid Dynamics Modeling of Extrathoracic Airway Flush: Evaluation of High Flow Nasal Cannula Design Elements. J Pulm Respir Med 6:376. doi: 10.4172/2161-105X.1000376Read Full Text Unlike NiPPV, HVNI is an open system de-escalation therapy—it is safe to turn on high and stabilize the patient fast. The clinician can then titrate down upon patient response.
No Additional Risk of Intubation with HVNI
In a multi-center, randomized, controlled trial conducted by Doshi and colleagues HVNI was shown to have equivalent outcomes to NiPPV in terms of intubation risks.55. Doshi, Pratik et al. High-Velocity Nasal Insufflation in the Treatment of Respiratory Failure: A Randomized Clinical Trial. Annals of Emergency Medicine, 2018. Published online ahead of print. https://www.ncbi.nlm.nih.gov/pubmed/29310868Read Full Text The study design randomized adults presenting in the emergency department with undifferentiated respiratory distress to a HVNI or NiPPV arm and followed them for 72 hours. The removal of CO2 from the blood is an important marker of ventilatory success, and Figure 1 depicts the comparison between HVNI and NiPPV.
Hi-VNI Technology
efficiently reduces CO2
Figure 1. Hi-VNI Technology Efficiently Reduces CO2
There was no significant difference between the reduction of CO2 between HVNI and NiPPV, and both show a significant drop in CO2 over time. In other words, HVNI is a viable alternative to NiPPV in providing ventilatory support to patients in undifferentiated respiratory distress, including hypercapnia or hypoxemia.
And thus, the simple answer to the question of whether you can achieve alveolar ventilation without pressure is: yes. HVNI.
HVNI Rated More Highly by Clinicians
One aspect in which the two modalities are not so similar is that HVNI is delivered through a mask-free interface via Hi-VNI® Technology, reducing the discomfort many patients experience with NiPPV. The patients can eat, drink, speak, and take oral medications. Clinicians rated patient response and comfort more highly with HVNI as compared to NiPPV.55. Doshi, Pratik et al. High-Velocity Nasal Insufflation in the Treatment of Respiratory Failure: A Randomized Clinical Trial. Annals of Emergency Medicine, 2018. Published online ahead of print. https://www.ncbi.nlm.nih.gov/pubmed/29310868Read Full Text
References